
A year ago on December 14, 2020 I began as a Registry Chaplain at a major hospital in the Atlanta area. Like so many families in 2020 our income was suddenly stopped. Both my husband and I do freelance work most of which relies on face-to face meetings. My husband is a photographer and I do project work in the nonprofit sector. When face-to-face gatherings suddenly ended in 2020, I was faced with finding another source of income. Hospital chaplaincy appeared to be my best option and one I’ve felt called to for years.
I applied to every opening in the greater Atlanta area. By October of 2020 I began to schedule interviews with three different major hospital systems. In November I was hired as a Registry Chaplain, which is PRN (as needed) work. As it turns out I am working 20-30 hours a week regularly, very good for PRN work.
The past year has been a whirlwind. In some ways it has passed quickly, but in others I feel like I’ve aged years. At the hospital where I work chaplains handle the decedent paperwork in addition to being a caring presence for the families of the deceased. This means we give the medical staff the death certificate worksheet to complete, make initial calls to both Lifelink and on occasion the Medical Examiner. We also are the main contact for the families when they decide on a funeral home. When a patient is near death a chaplain is often called to be with the patient and their family. The total time with the patient and family and then to complete the paperwork can vary between 2 – 4 hours before during and after a death to the completion of the paperwork.
Since December of 2020 as a part-time chaplain I’ve handled the decedent paperwork for 76 patients. At my one year anniversary I was curious how many people I had handled this for in less than 120 days of work, so I went through our log book and counted. I needed to see the proof as to why I felt so heavy.
Early on in my time at the hospital I was trying to get as may hours as I could in an effort to make up some lost ground in our household income. All was going well until somewhere in mid-February I hit a major wall. I felt awful and was thoroughly checked out medically. I realized I felt awful because of the shear numbers of dead and dying patients and their families I had met with in a few short months. In one 12 hour shift in January of 2021 I had 6 deaths. In that 12 hour period I had no time for even a sip of water or a bite of food. It was at this time I learned to take breaks as I could. Often taking quick breaks to eat a protein bar or drink water. I no longer packed my schedule.
The need for self-care is not optional in this work. Writing about the things I’ve learned is one way for me to take care of myself. My hope is that my reflections will help others who find themselves in this reflection and take time for self-care.
A few random things I’ve learned in the past year in not particular order:
- Our healthcare workers are true heroes.
- I watched the medical staff in more Code Blue situations than I can count. It is an amazing situation to watch. Scores of people descend on a room and each knows their role, and what is expected of them. This is team work in literal life and death situations. I am left in awe each time I report to a code.
- I was surprised to find over the past year the number of nurses, doctors, physician assistants and nurse practitioners who will tell us, the chaplains, they couldn’t do our job.
- Related to the point above, healthcare and the fire service is similar. At a fire scene as chaplain I go to the family to comfort them as they watch smoke and flames billow out of their home. The firefighters tell me they couldn’t do what I do, but they walk into the flames. I cannot do what the firefighters do nor what the nurses at the hospital do. We each have our role to play and are highly trained to do it.
- Nothing will frustrate an ICU or CCU medical team more than a family who will go against the patients wishes and not make them DNR (do not resuscitate). The medical team knows that at a certain point keeping a person’s heart beating does not mean they will get better and go home. Many times it just prolongs the suffering of the patient. It is far more compassionate to let a natural death to occur. See THIS article about doctors and end of life care.
- Another frustrating thing for medical workers is the spreading of false information and conspiracy theories. Just don’t do it. People are losing their lives because they are not vaccinated.
- Medical staff is often left with many questions when a family who professes a faith in God, and the belief that life does not end, but that a faithful person will live on with God, prevents their loved one from that hopeful death.
- In the midst of some really awful days, sharing a photo of a new baby or puppy can really brighten the moment.
- The funeral homes and their transportation people are also feeling the stress from the pandemic. Did you know there is a whole business just to pick up deceased patients and take them to the preferred funeral home? While the pandemic may be good for these businesses the people who work for these businesses are feeling the strain too.
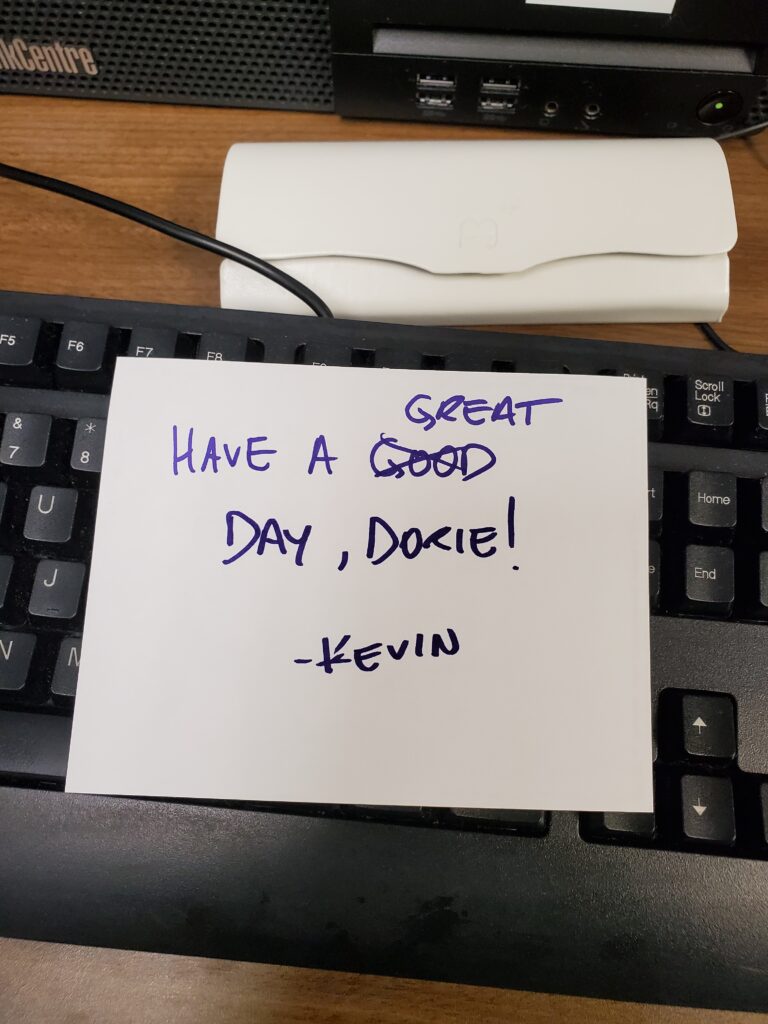
- Hospital staff appreciate people in the community sending in treats. Hearing thank you helps.
- Hospital administration, at least at our hospital, work very hard at finding ways in which to support the staff. Their work is a different type of tough with it’s own set of stressors.
- Humor is a great stress reliever. I learned that when my oldest son was to be commissioned in the Army then again before his deployment to Afghanistan. I took a comedy writing class before each of those events. The lessons learned in those classes has seen me through some difficult experiences since. You can see the graduation videos Here and Here.
- I work with some amazing people in the pastoral care office. It is so refreshing, and rare, to work with a team of professionals who support each other.
- The role of a chaplain is misunderstood by many. A hospital chaplain is trained to listen, be present and help people access their own means of support. We are a caring presence for people at some of the toughest times of their lives. At the core of being a chaplain is being present for people going through a tough time. We can’t change what is happening but we can let a person know they are not alone at a time they may feel completely deserted.
I am sure I’ll think of other lessons from the past year, but for now these are the ones I’ve had on my mind. As we battle the latest variant of the virus and continue to battle misinformation, I’m sure I’ll feel the need to write again.
A few photos follow of some pretty neat things that happened the past year.

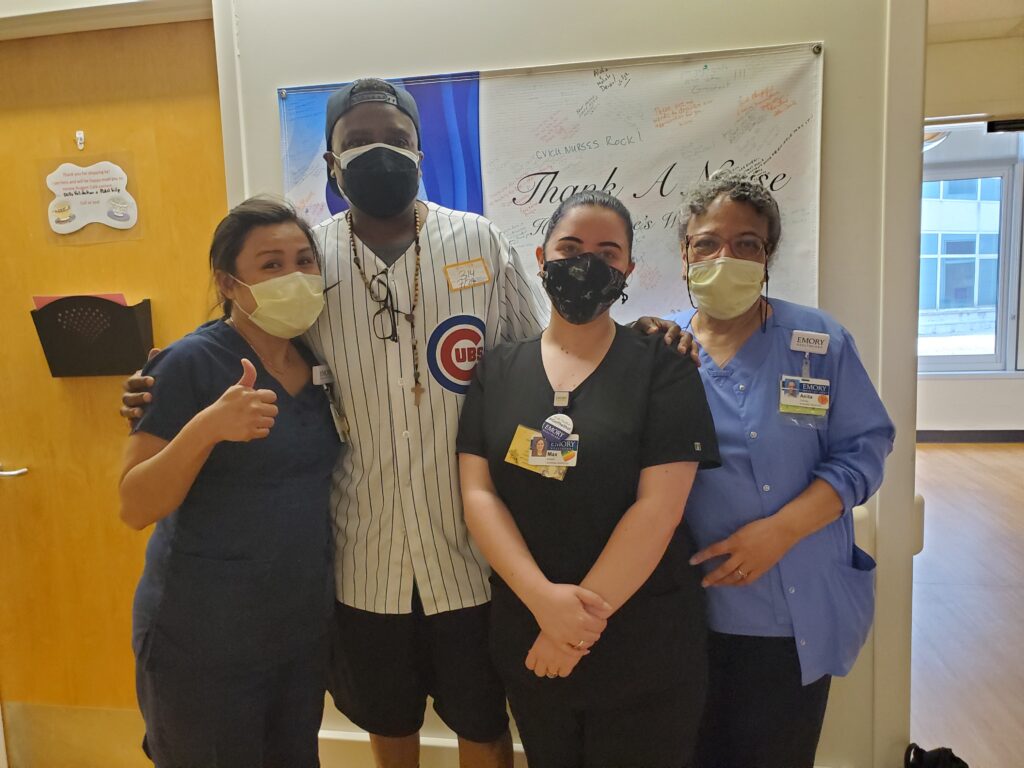
Jason Weaver took extra time to visit with some of my work family, Tiffany, Max and Anita.
